Everest House Surgery
Everest Way, Hemel Hempstead, Herts, HP2 4HY
Telephone: 01442 500 164
Sorry, we're currently closed. Please call NHS 111

Closure of Everest House Pharmacy Local Health Services Extremely Busy Young People’s Event Pharmacy First You can now see and access your prescriptions electronically in the NHS App….. NHS Jewish BRCA Testing Programme Measles Infection Booking an Appointment for a Blood Test MMR Vaccine – Protect Yourself and Your Family Clinical System Outage – Monday 11th and Tuesday 12th of December
Cervical Screening Information
It is your choice whether to have a cervical screening test or not. This guidance aims to help you decide. Cervical screening used to be called a ‘smear test’.
Please find below information on cervical screening. If you require this information in a different language this information is available at the bottom of this page.
Why we offer cervical screening
NHS cervical screening helps prevent cervical cancer. It saves thousands of lives from cervical cancer each year in the UK. In England cervical screening currently prevents 70% of cervical cancer deaths. If everyone attended screening regularly, 83% could be prevented.
Who we invite
Cervical screening is for women and people with a cervix. We offer screening every 3 years from age 25 to 49 and every 5 years from age 50 to 64. This is because most cervical cancers develop between these ages. First invitations arrive a few months before people turn 25. You can book your appointment as soon as you get your invitation. We invite some people more often due to a previous screening result (see below).
You should consider having screening regardless of your sexual orientation, sexual history, or whether you have had the human papillomavirus (HPV) vaccination.
If you are a transgender (trans) man registered as female, we will send you invitations for cervical screening. If you are registered as male you won’t receive invitations, but we can arrange an appointment for you if you have a cervix. If you are a trans woman you don’t need cervical screening.
Info for the Transgender and Non-Binary Communities
If you are a trans man or identify as non-binary, you may still be at risk for certain gynecological cancers if you have retained any reproductive organs, such as the womb, cervix, ovaries, fallopian tubes, vagina, or vulva. It’s important to be aware of potential symptoms and to take steps to maintain your gynecological health.
If you still have a cervix and have not yet undergone cervical screening—or believe you may be due for one—please call the surgery to book an appointment with one of our nurses. With your consent, we can register you in the Cervical Screening Management System to ensure you receive automatic reminders for future screenings.
Click the link below for more information.
Info for the Transgender and Non-binary Communities | The Eve Appeal
Cervical cancer
Cervical cancer happens when cells in the cervix grow in an uncontrolled way and build up to form a lump (also called a tumour). As the tumour grows, cells can eventually spread to other parts of the body and become life-threatening.
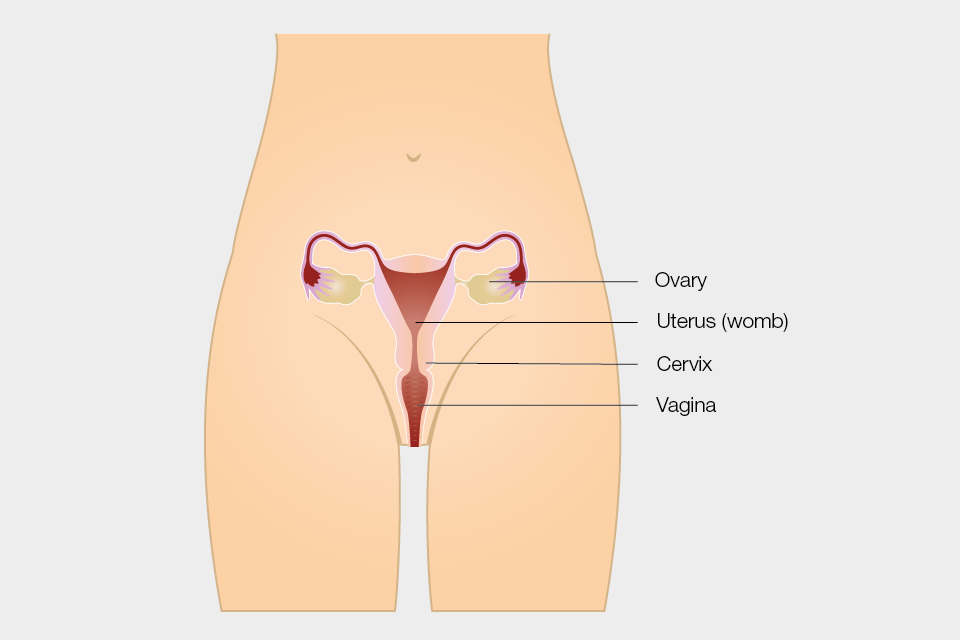
Your cervix is the lowest part of your uterus (or womb), and it is found at the top of your vagina.
HPV and cervical cancer
Nearly all cervical cancers are caused by a virus called human papillomavirus (HPV).
HPV is very common. Most people will get the virus at some point in their life. It is spread through close skin to skin contact during any type of sexual activity with a man or woman. HPV can stay in the body for many years. It can stay at very low or undetectable levels and not cause any problems. This means an HPV infection may have come from a partner a long time ago.
There are many different types of HPV, but only some high-risk types can lead to cancer. The types of HPV that cause cervical cancer do not cause any symptoms. In most cases, your immune system can get rid of the virus without you ever knowing you had it. But sometimes, HPV can cause cells in your cervix to become abnormal.
Your body can usually get rid of the abnormal cells and your cervix returns to normal. But sometimes this doesn’t happen, and the abnormal cells can go on to develop into cancer.
What affects your chances of getting cervical cancer
Having cervical screening lowers your chances of getting cervical cancer. Screening finds abnormal cells so they can be removed before they become cancer.
HPV is found on the skin around the whole genital area and can be spread through any type of sexual activity. This means that condoms or dental dams can help prevent infection, but they don’t provide total protection from HPV.
Smoking increases the risk of cervical cancer because it makes it harder for your body to get rid of HPV infections. Information about stopping smoking is available on the NHS smokefree website.
The HPV vaccination protects against the types of high-risk HPV that cause most cervical cancers. If you have had the HPV vaccination you will still need to consider having cervical screening when you are invited. This is to check for other high-risk HPV types that can lead to cervical cancer.
Having a family history of cervical cancer does not affect your chances of developing cervical cancer.
How cervical screening works
Cervical screening is not a test for cancer. It looks for abnormal cells in the cervix. Abnormal cells can develop into cancer if left untreated.
The test involves using a soft brush to take a small sample of cells from the surface of your cervix. The sample is put into a small plastic container and sent to a laboratory. It is tested for the types of HPV that can cause cervical cancer. If you have a negative result for the most common types of HPV that cause cervical cancer, your risk of cervical cancer is very low and there is no need to check for abnormal cells even if you have had these in the past.
If you have a positive result for HPV we will check the sample for abnormal cells. Abnormal cells are not cancer, but they could develop into cancer if left untreated.
As a next step we may offer you another examination (called a colposcopy) to look at your cervix more closely. If we find abnormal cells during colposcopy we may suggest you have the cells removed. This is how screening can prevent cervical cancer.
No screening test is 100% effective
In cervical screening this is because:
- an HPV infection or abnormal cells can sometimes be missed (a ‘false negative’ result)
- abnormal cells can develop and turn into cancer in between screening tests
- there is a small chance that a result says abnormal cells are found when the cervix is normal (a ‘false positive’ result)
If screening does not find abnormal cells this does not guarantee that you do not have them, or that they will never develop in the future.
Having cervical screening
Before your appointment
Cervical screening is usually carried out by a female nurse here at the practice.
Your appointment should be on a day when you are not having a period. If you don’t have periods, you can be screened at any time.
Please don’t use any vaginal medications, lubricants or creams in the 2 days before you have your test because they can affect the results.
Please talk to your nurse or doctor if you:
- are pregnant
- have had a hysterectomy
- think it would be difficult for you to have the test
You can speak to your nurse or doctor if you are nervous about screening. They can talk through any questions or concerns you have. If you decide to go ahead with screening, they can make arrangements to help you feel more comfortable.
At your appointment
The actual test only takes 1 to 2 minutes. The whole appointment usually takes about 10 minutes.
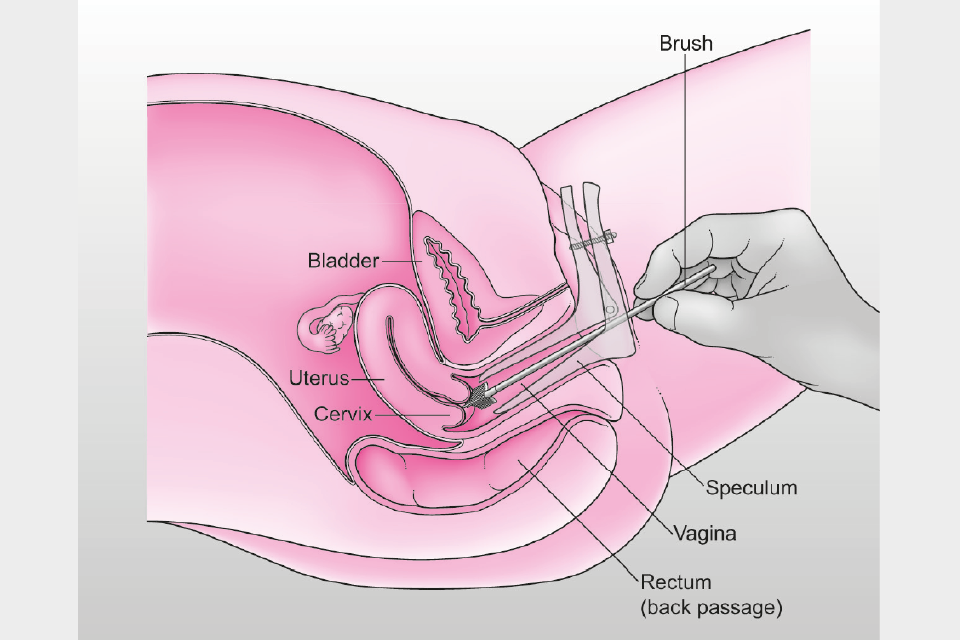
The nurse will ask you to undress from your waist down (or just remove your underwear if you are wearing a loose skirt) and lie on a bed with your knees bent and apart. You will have a paper sheet or towel to cover your stomach and hips.
They will put a device called a speculum into your vagina and open it gently. This allows them to see your cervix. The speculum is usually made of plastic and a new one is used for each screening test. The nurse or doctor then uses a small soft brush to take a sample of cells from the surface of your cervix. You might feel some discomfort, but this should go away quickly. If it feels painful, tell the nurse or doctor and they will try to make it more comfortable for you.
You are in control of your screening appointment, and you can ask to stop at any time.
Cervical screening results
The nurse will tell you when you can expect your results letter. There are 4 possible results.
1. HPV negative
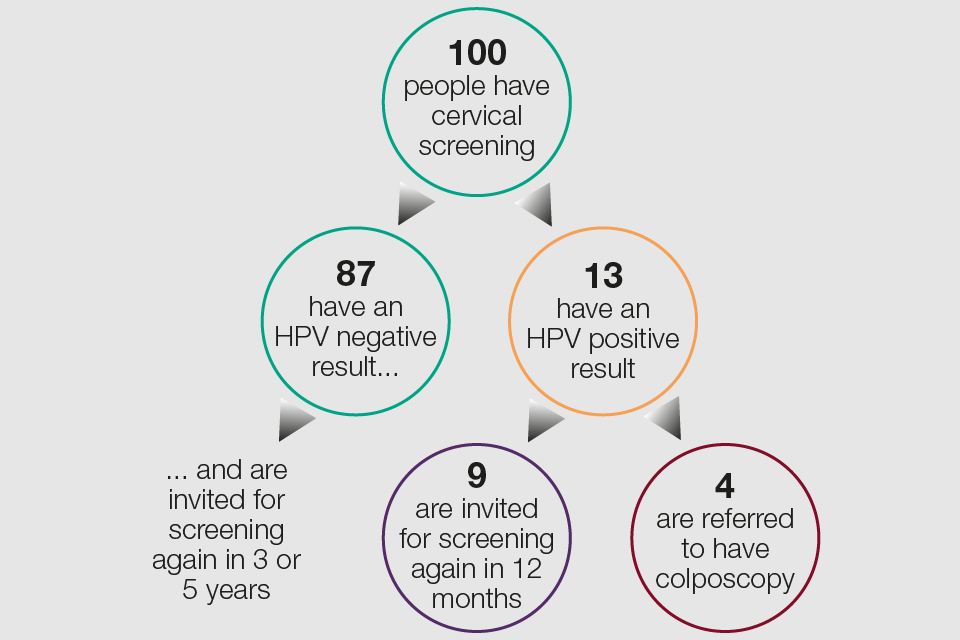
An HPV negative result means we will not do any further tests. This result means it is highly unlikely that you will have any abnormal cervical cells. Even if you did, it would be extremely unlikely that they would cause a problem. We will simply call you back for screening again in 3 or 5 years’ time (depending on your age).
2. HPV positive: no abnormal cells
If your sample is HPV positive we also test it for abnormal cervical cells. If none are found, your result will say you have HPV, but no abnormal cells. We will ask you to come for screening again sooner than usual (your result letter will explain when). This is so we can check if your immune system has got rid of the HPV (this happens in most cases).
3. HPV positive: abnormal cells found
There are several ‘grades’ of abnormal cells as some are more serious than others. Your result letter will explain what your results mean. If you have HPV and any grade of abnormal cervical cells we will refer you for colposcopy (see information below). We will send you our information leaflet NHS cervical screening – having a colposcopy.
4. Inadequate result
Occasionally a sample may be called ‘inadequate’. This may be due to a technical problem, for example, if the laboratory cannot get an HPV test result from your sample or cannot see if abnormal cells are present or not. If you have an inadequate test, we will ask you to have cervical screening again in 3 months’ time. We wait so that there are enough cells again to get a sample from.
If you require this information in a different language please click here.









